In a prospective study, researchers used quantitative magnetic resonance cholangiopancreatography (MRCP) to monitor changes in bile duct disease over time. The study tracked 55 patients with primary sclerosing cholangitis (PSC), demonstrating that quantitative MRCP metrics, obtained through MRCP+ by Perspectum, could detect subtle changes in ductal disease that were not apparent through traditional imaging or biochemical markers. A total of 92 quantitative MRCP+ metrics were calculated for each participant, of which 24 were selected to assist in identifying patients with PSC. The findings indicate that quantitative MRCP+ can distinguish PSC from healthy controls and other immune-mediated liver diseases. This work thus showcases the potential of quantitative MRCP+ as a tool for enhancing the diagnostic and prognostic accuracy in managing PSC.
Read full study
Quantitative MRCP and metrics of bile duct disease over time in patients with primary sclerosing cholangitis: A prospective study
Alimentary Pharmacology & Therapeutics, 2024
Abstract
Objective: Imaging markers of biliary disease in primary sclerosing cholangitis (PSC) have potential for use in clinical and trial disease monitoring. Herein, we evaluate how quantitative magnetic resonance cholangiopancreatography (MRCP) metrics change over time, as per the natural history of disease.
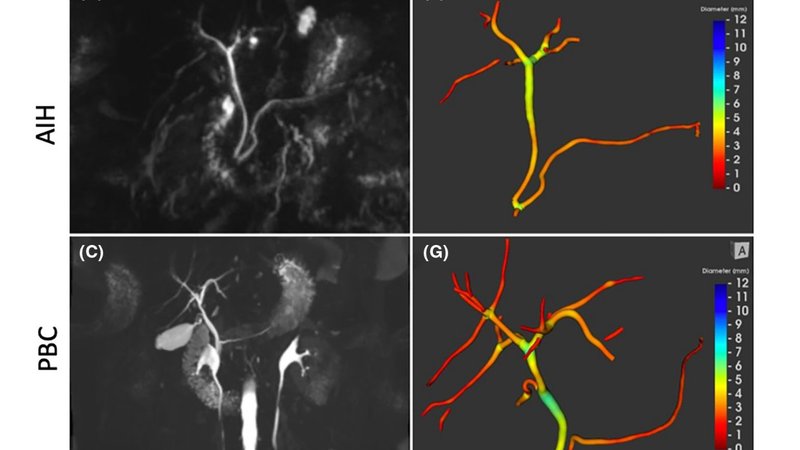
Materials and methods: Individuals with PSC were prospectively scanned using non-contrast MRCP. Quantitative metrics were calculated using MRCP+ post-processing software to assess duct diameters and dilated and strictured regions. Additionally, a hepatopancreatobiliary radiologist (blinded to clinical details, biochemistry and quantitative biliary metrics) reported each scan, including ductal disease assessment according to the modified Amsterdam Cholangiographic Score (MAS).
Results: At baseline, 14 quantitative MRCP+ metrics were found to be significantly different in patients with PSC (N = 55) compared to those with primary biliary cholangitis (N = 55), autoimmune hepatitis (N = 57) and healthy controls (N = 18). In PSC specifically, baseline metrics quantifying the number of strictures and the number and length of bile ducts correlated with the MAS, transient elastography and serum ALP values (p < 0.01 for all correlations). Over a median 371-day follow-up (range: 364-462), 29 patients with PSC underwent repeat MRCP, of whom 15 exhibited quantitative changes in MRCP+ metrics. Compared to baseline, quantitative MRCP+ identified an increasing number of strictures over time (p < 0.05). Comparatively, no significant differences in biochemistry, elastography or the MAS were observed between timepoints. Quantitative MRCP+ metrics remained stable in non-PSC liver disease.
Conclusion: Quantitative MRCP+ identifies changes in ductal disease over time in PSC, despite stability in biochemistry, liver stiffness and radiologist-derived cholangiographic assessment (trial registration: ISRCTN39463479).
